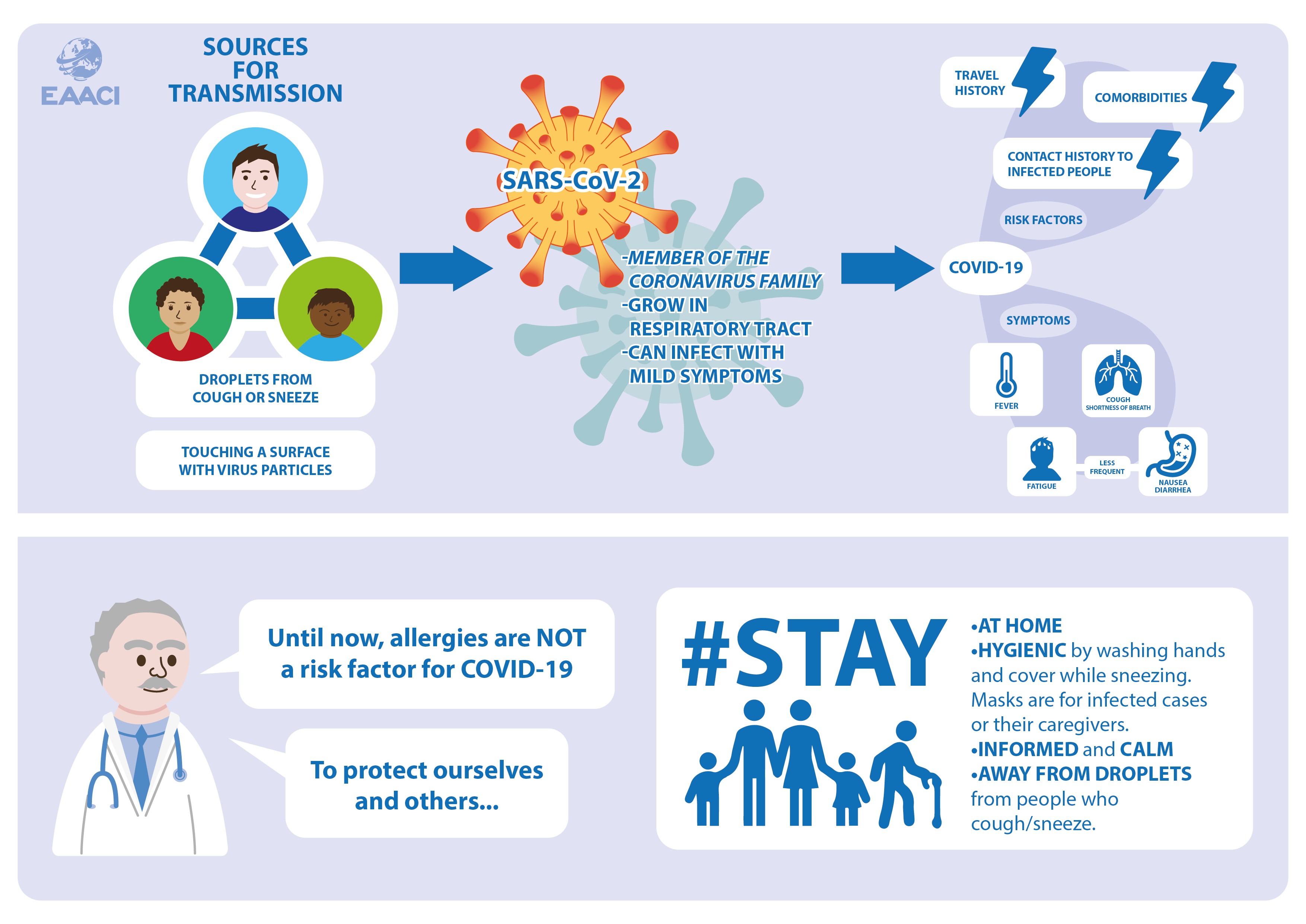
Starting from December 2019, a new strain of human coronavirus was detected, initially called 2019-nCoV, in few patients with viral pneumonia in Wuhan, China. This new virus was officially called SARS-CoV-2 (severe acute respiratory coronavirus 2), while the disease caused by SARS-CoV-2 was named COVID-19 (coronavirus disease 2019).
Since its first appearance in humans, SARS-CoV-2 is spreading worldwide, with more than 950,000 cases (updated on March 27th) distributed in many countries in Asia, America, Europe, Australia, and Africa. The World Health Organization (WHO) has declared the COVID-19 outbreak a global pandemic and is monitoring its dynamics closely. To provide a summary of the current situation, we have reviewed and summarized the latest scientific publications.
What is the Coronavirus?
Coronaviruses are enveloped RNA viruses, named for the crown or corona-like appearance of the envelope glycoproteins. These spike glycoproteins allow the virus to attach and inject genetic material into host cells to infect them. SARS-CoV-2 appears to replicate efficiently in the upper respiratory tract, which means that the virus load increases. Mild symptoms hardly interfere with everyday routines, although infected individuals can already produce a large number of viruses and infect other people. The virus replicates also in the lungs, which can be seen in images produced for example by x-ray or computed tomography. In the blood, mainly the reaction of the immune system to the virus can be observed via formation of antibodies.
Where did the virus come from and how is it transmitted?
COVID-19 belongs to the group of zoonotic diseases, caused by germs passing from animals to humans. The precise origin of SARS-CoV-2 has not yet been determined. SARS-CoV-2 can be transmitted through respiratory droplets produced through coughing/sneezing, and by directly touching eyes, noses after touching any surface/object with the virus on it. However, we still lack detailed information on how long the virus can survive on surfaces. Fortunately, SARS-CoV-2 is not passed from mother to child or through breastfeeding.
How is COVID-19 diagnosed?
Two important aspects need to be combined in order to raise a suspicion of COVID-19:
- any contact to persons with a confirmed infection with SARS-CoV-2, and/or a travel history to risk areas or countries with confirmed cases.
- Symptoms frequently associated with COVID-19, such as:
- Fever
- Respiratory symptoms (mainly dry cough, and shortness of breath)
Fatigue and gastrointestinal symptoms such as nausea, diarrhea can also be associated with COVID-19.
The precise diagnosis is confirmed in symptomatic patients when SARS-CoV-2 is detected in specific samples of a patient. Usually, throat swabs are being tested, but also other samples like sputum may serve to detect the virus. A technique called reverse transcriptase-polymerase chain reaction is used to detect the virus’s genetic material in samples. Available tests based on specific antibody measurement are not suitable for SARS-CoV-2 detection.
What is the course of COVID-19 once a patient is infected?
Generally, symptoms caused by coronavirus infection are mild. However, some of the patients may develop severe respiratory disease, kidney failure, septic shock, or even death. Chronic illness such as hypertension and diabetes mellitus were the most frequent comorbid disease in severe cases.
Is COVID-19 treatable?
Although a specific treatment is currently still unavailable, physicians have several options to help patients by managing symptoms with drugs and supportive systems.
Further, Infection Prevention Control (IPC) measures at home for both suspected patients and relatives/caregivers are being implemented widely. For instance, a frequent hand hygiene regime, a distance (at least 1 meter) between these subjects, the use of medical masks when in the same room, and maintenance of airflow by opening windows.
What can we do to protect ourselves and others?
While vaccines for coronavirus are still being developed, everybody can actively protect himself/herself and others by:
- following your country´s regulations to reduce virus transmission (e.g. by staying at home and reducing social contacts as much as possible)
- implementing standard hygiene measures such as covering the mouth with a disposable tissue or the elbow when sneezing/coughing.
- using masks only for those who are infected with SARS-Co-V-2 and need to be for instance transported from one place to somewhere else, or for those who look after the infected people.
- avoiding close contacts with patients with respiratory symptoms
- WASH YOUR HANDS frequently!
Lastly, it’s important to stay informed but remain calm. Outbreaks of infectious diseases can be scary and affect our mental health. The following websites provide information on how to support and manage our wellbeing during such times.
https://www.who.int/emergencies/diseases/novel-coronavirus-2019
Does asthma predispose for COVID-19?
Viral infections are well-known risk factors for an exacerbation of asthma. In the study by Yang et al., 40% of the COVID-19 patients with critical symptoms had an underlying long-term disease before the infection. Another study of 140 cases from Wuhan (China) did not report allergic diseases as co-morbidities among severe cases. However, more information needs to be gathered and analyzed to create reliable reports on risk factors for severe COVID-19.
References:
- Yang X, Yu Y, Xu J, Shu H, Xia Ja, Liu H, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med 2020.
- Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet 2020; 395: 565–74.
- Phan LT, Nguyen TV, Luong QC, Nguyen TV, Nguyen HT, Le HQ, et al. Importation and Human-to-Human Transmission of a Novel Coronavirus in Vietnam. N Engl J Med. 2020.
- World Health Organization. Coronavirus disease 2019 (COVID-19) Outbreak. Link: https://www.who.int/emergencies/diseases/novel-coronavirus-2019
- COVID-19 Resource Centre. The Lancet. Link: https://www.thelancet.com/coronavirus
- Zhang JJ, Dong X, Cao YY, Yuan YD, Yang YB, Yan YQ, Akdis CA, Gao YD. Clinical characteristics of 140 patients infected by SARS-CoV-2 in Wuhan, China. Allergy. 2020 Feb 19. doi: 10.1111/all.14238. [Epub ahead of print]
- Heyman DL, Shindo N. COVID-19: what is next for public health?February 22, 2020. Vol 395: 542-545.
- Woelfel R, Corman VM, Guggemos W et al. Clinical presentation and virological assessment of hospitalized cases of coronavirus disease 2019 in a travel-associated transmission cluster. medRxiv 2020.03.05.20030502; doi: https://doi.org/10.1101/2020.03.05.20030502.
- Xu Y, Li X, Zhu B et al. Characteristics of pediatric SARS-CoV-2 infection and potential evidence for persistent fecal viral shedding. Nat Med 2020. https://doi.org/10.1038/s41591-020-0817-4.
EAACI blog initiative
Author: Tu HK Trinh (University of Medicine and Pharmacy at Ho Chi Minh City, Vietnam). 
Tu is an allergist, postdoctoral researcher at the group of Allergy-Clinical Immunology at the Center for Molecular Biomedicine. She completed her Ph.D. in Ajou University (South Korea) looking at novel therapies and biomarkers for asthma phenotypes with Prof.Hae-Sim Park. Back to Vietnam, her aim is to bring up the current diagnostic and treatments tools for allergic patients there, and to build up a fully functional laboratory for clinical translational research covering allergy/immunology field. She is a steering committee member of WAO JM, APAPARI JM and HSAACI.
Mentor:
Dr.Paula Kauppi, MD, PhD, Adj Prof., Department of Allergy, Inflammation Center, Helsinki University Hospital, Helsinki Finland.
Dr.Juha Jantunen, PhD, Researcher, South Karelia Allergy and Environment Institute, Imatra, Finland.