Vaccination protects against measles, tuberculosis, influenza and a vast array of other diseases. It has been proven to save millions of lives worldwide and is therefore an indispensable public health measure.
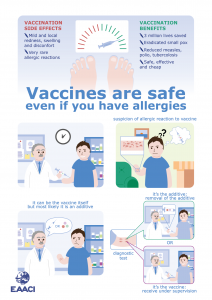
Nearly all medicines have potential side effects; those most commonly observed for vaccination are non-serious, and include slight pain and fever, swelling, or redness around the injection site.
In a very small number of cases (less than 1 in 100,000) there is a suspicion that a vaccine may have induced a serious allergic reaction, especially in individuals with pre-existing allergies.
The EAACI position paper on “Vaccination and allergy” discusses the low risk of allergic reactions from vaccination in allergic individuals, and how it can be further reduced.
Your allergic status alone should never rule out vaccination
Today’s vaccines are made of several different ingredients, designed to be as safe and effective as possible. Each ingredient serves a specific purpose: providing immunity, keeping the vaccine long lasting, or preventing contamination.
It is important to note that allergic responses to vaccines are usually directed against vaccine additives, rather than the main ingredients of the vaccine.
Therefore, knowing the full composition of a vaccine formulation is crucial for allergy diagnosis. Currently, lab tests for allergic responses to vaccine components cannot predict an allergic response, and hence are not recommended.
However, due to the low level of risk of allergic responses to vaccines even in people with one or multiple allergies, the allergic status alone should never rule out vaccination.
Instead, vaccination is often possible for patients allergic to foods or other environmental allergens even without any precautions and in the outpatient clinic.
If an allergic response at the injection site is observed by yourself or your doctor after vaccination, the additive that the allergic response is directed to can be identified by allergen skin prick test.
Once identified, the next vaccinations should use vaccine preparations without the offending additive. Only in those very few patients with allergist-confirmed allergy to the vaccine or its components, where the vaccine required contains a relevant amount of the allergen, vaccination should be given under medical supervision, so that the small risk of a serious allergic reaction can be safely managed.
No association between vaccination and development of allergies
In addition, there has been concern by patients that stimulation of the immune system by vaccination could increase the risk of developing further allergies in children, a number of well-controlled clinical trials deny such association.
Therefore, vaccination does not increase the risk of developing other allergic diseases, has a minimal risk of causing a severe allergic reaction (which can be managed in a clinical setting), and presents a dramatic benefit to human health.
References
Vaccination and allergy: EAACI position paper, practical aspects, Lennart Nilsson; Knut Brockow; Johan Alm; Victoria Cardona; Jean‐Christoph Caubet; Eva Gomes; Maria C. Jenmalm; Susanne Lau; Eva Netterlid; Jürgen Schwarze; Aziz Sheikh; Jann Storsaeter; Chrysanthi Skevaki; Ingrid Terreehorst; Giovanna Zanoni; First published: 04 August 2017 https://doi.org/10.1111/pai.12762